In the spring of 2013, I flew to San Diego to one of the most provocative meetings that I have ever attended. Entitled ‘The Future of Genomic Medicine’, the meeting was at the Scripps Institute in La Jolla, at a conference centre overlooking the ocean. The site was a monument to modernism—blond wood, angular concrete, mullions of steel. The light on the water was blindingly glorious. Joggers with post-human bodies ran lankily across the boardwalk. The population geneticist David Goldstein spoke about ‘Sequencing Undiagnosed Conditions of Childhood’, an effort to extend massively parallel gene sequencing to undiagnosed childhood diseases. The physicist-turned-biologist Stephen Quake discussed the ‘Genomics of the Unborn’, the prospect of diagnosing every mutation in a growing foetus by sampling the scraps of foetal DNA that spill naturally into maternal blood.
On the second morning of the conference, a 15-year-old girl—I’ll call her Erika—was wheeled onstage by her mother. Erika wore a lacy, white dress and had a scarf slung across her shoulders. She had a story to tell—of genes, identity, fate, choices, and diagnosis. Erika has a genetic condition that has caused a severe, progressive degenerative disease. The symptoms began when she was one-and-a-half years old—small twitches in her muscles. By four, the tremors had progressed furiously; she could hardly keep her muscles still. She would wake up 20 or 30 times every night, drenched in sweat and racked by unstoppable tremors. Sleep seemed to worsen the symptoms, so her parents took shifts to stay awake with her, trying to console her into a few minutes of rest every night.
Clinicians suspected an unusual genetic syndrome, but all known genetic tests failed to diagnose the illness. Then in June 2011, Erika’s father was listening to National Public Radio when he heard about a pair of twins in California, Alexis and Noah Beery, who also had a long history of muscle problems. The twins had undergone gene sequencing and ultimately been diagnosed with a rare new syndrome. Based on that genetic diagnosis, the supplementation of a chemical, 5-hydroxytryptamine, or 5-HT, had dramatically reduced the twins’ motor symptoms.
Erika hoped for a similar outcome. In 2012, she was the first patient to join a clinical trial that would attempt to diagnose her illness by sequencing her genome. By the summer of 2012, the sequence was back: Erika had not one but two mutations in her genome. One, in a gene called ADCY5, altered nerve cells’ capacity to send signals to each other. The other was in a gene, DOCK3, that controls nerve signals that enable the coordinated movement of muscles. The combination of the two had precipitated the muscle-wasting and tremor-inducing syndrome. It was a genetic lunar eclipse—two rare syndromes superposed on each other, causing the rarest of rare illnesses.

In the 1920s in the US, doctors chose ‘healthy’ babies in ‘Better Baby’ fetes
After Erika’s talk, as the audience spilled into the lobby outside the auditorium, I ran into Erika and her mother. Erika was utterly charming—modest, thoughtful, sober, mordantly funny. She seemed to carry the wisdom of a bone that has broken, repaired itself, and become stronger. She had written a book and was working on another. She maintained a blog, helped raise millions of dollars for research, and was, by far, among the most articulate, introspective teenagers that I have ever encountered. I asked her about her condition, and she spoke frankly of the anguish it had caused in her family. “Her biggest fear was that we wouldn’t find anything. Not knowing would be the worst thing,” her father once said.
But has “knowing” altered everything? Erika’s fears have been alleviated, but there is very little that can be done about the mutant genes or their effects on her muscles. In 2012, she tried the medicine Diamox, known to alleviate muscle twitching in general, and had a brief reprieve. There were 18 nights of sleep—a lifetime’s worth for a teenager who had hardly experienced a full night’s sleep in her life—but the illness has relapsed. The tremors are back. The muscles are still wasting away. She is still in her wheelchair.
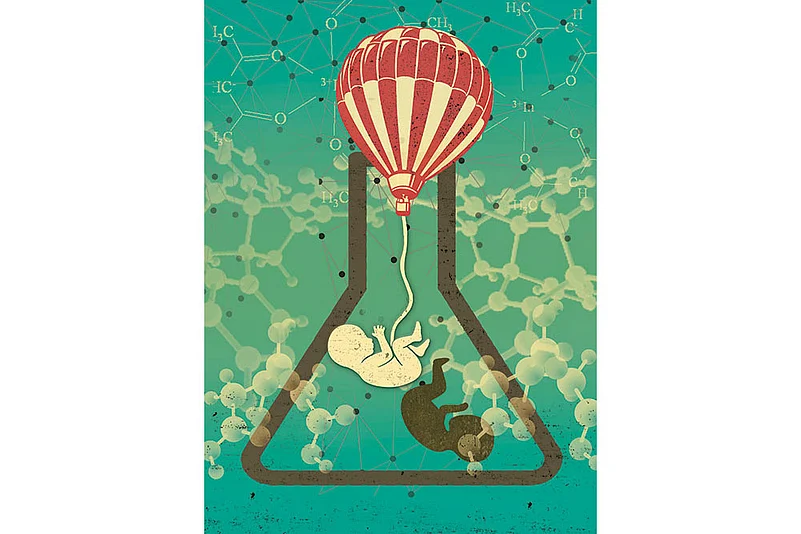
What if we could devise a pre-natal test for this disease? Stephen Quake had just finished his talk on foetal genome sequencing—on “the genetics of the unborn”. It will soon become feasible to scan every foetal genome for all potential mutations and rank many of them in order of severity and penetrance. We do not know all the details of the nature of Erika’s genetic illness—perhaps, like some genetic forms of cancer, there are other, hidden “cooperative” mutations in her genome—but most geneticists suspect that she has only two mutations, both highly penetrant, causing her symptoms.

Dylan
Should we consider allowing parents to fully sequence their children’s genomes and potentially terminate pregnancies with such known devastating genetic mutations? We would certainly eliminate Erika’s mutation from the human gene pool—but we would eliminate Erika as well. I will not minimise the enormity of Erika’s suffering, or that of her family—but there is, indubitably, a deep loss in that. To fail to acknowledge the depth of Erika’s anguish is to reveal a flaw in our empathy. But to refuse to acknowledge the price to be paid in this trade-off is to reveal, conversely, a flaw in our humanity.
A crowd was milling around Erika and her mother, and I walked down toward the beach, where sandwiches and drinks were being laid out. Erika’s talk had sounded a resonantly sobering note through a conference otherwise tinged with optimism: you could sequence genomes hoping to find match-made medicines to alleviate specific mutations, but that would be a rare outcome. Pre-natal diagnosis and the termination of pregnancies still remained the simplest choice for such rare devastating diseases—but also ethically the most difficult to confront. “The more technology evolves, the more we enter unknown territory. There’s no doubt that we have to face incredibly tough choices,” Eric Topol, the conference organiser, told me. “In the new genomics, there are very few free lunches.”
Indeed, lunch had just ended. The bell chimed, and the geneticists returned to the auditorium to contemplate the future’s future. Erika’s mother wheeled her out of the conference centre. I waved to her, but she did not notice me. As I entered the building, I saw her crossing the parking lot in her wheelchair, her scarf billowing in the wind behind her, like an epilogue.
Let’s turn to the question: How much of the human genome can we “read” in a usable or predictive sense? Until recently, the capacity to predict fate from the human genome was limited by two fundamental constraints. First, most genes, as Richard Dawkins describes them, are not “blueprints” but “recipes”. They do not specify parts, but processes; they are formulas for forms. If you change a blueprint, the final product is changed in a perfectly predictable manner: eliminate a widget specified in the plan, and you get a machine with a missing widget. But the alteration of a recipe or formula does not change the product in a predictable manner: if you quadruple the amount of butter in a cake, the eventual effect is more complicated than just a quadruply buttered cake (try it; the whole thing collapses in an oily mess). By similar logic, you cannot examine most gene variants in isolation and decipher their influence on form and fate. That a mutation in the gene MECP2, whose normal function is to add chemical modifications to DNA, may cause a form of autism is far from self-evident (unless you understand how genes control the neurodevelopmental processes that make a brain).

When Dylan a boxer, died, two clones were there to replace him
The second constraint—possibly deeper in significance—is the intrinsically unpredictable nature of some genes. Most genes intersect with other triggers—environment, chance, behaviours, or even parental and pre-natal exposures—to determine an organism’s form and function, and its consequent effects on its future. Most of these interactions, we have already discovered, are not systematic: they happen as a result of chance, and there is no method to predict or model them with certainty. These interactions place powerful limits on genetic determinism: the eventual effects of these gene-environment intersections can never be reliably presaged by the genetics alone. Indeed, recent attempts to use illnesses in one twin to predict future illnesses in the other have come up with only modest successes.
But even with these uncertainties, several predictive determinants in the human genome will soon become knowable. As we investigate genes and genomes more deftly, more comprehensively, and with more computational power, we should be able to “read” the genome more thoroughly—at least in a probabilistic sense. Currently, only highly penetrant single-gene mutations (Tay-Sachs disease, cystic fibrosis, sickle-cell anaemia), or alterations in entire chromosomes (Down syndrome), are used in genetic diagnosis in clinical settings. But there is no reason that the constraints on genetic diagnosis should be limited to diseases caused by mutations in single genes or chromosomes. Nor, for that matter, is there any reason that “diagnosis” be restricted to disease. A powerful enough computer should be able to hack the understanding of a recipe: if you input an alteration, one should be able to compute its effect on the product.
By the end of this decade, permutations and combinations of genetic variants will be used to predict variations in human phenotype, illness, and destiny. Some diseases might never be amenable to such a genetic test, but perhaps the severest variants of schizophrenia or heart disease, or the most penetrant forms of familial cancer, say, will be predictable by the combined effect of a handful of mutations. And once an understanding of “process” has been built into predictive algorithms, the interactions between various gene variants could be used to compute ultimate effects on a whole host of physical and mental characteristics beyond disease alone. Computational algorithms could determine the probability of the development of heart disease or asthma or sexual orientation and assign a level of relative risk for various fates to each genome. The genome will thus be read not in absolutes, but in likelihoods—like a report card that does not contain grades but probabilities, or a resume that does not list past experiences but future propensities. It will become a manual of previvorship.
In April 1990, as if to raise the stakes of human genetic diagnosis further, an article in Nature magazine announced the birth of a new technology that permitted genetic diagnosis to be performed on an embryo before implantation into a woman’s body.
The technique relies on a peculiar idiosyncrasy of human embryology. When an embryo is produced by in vitro fertilisation (IVF), it is typically grown for several days in an incubator before being implanted into a woman’s womb. Bathed in a nutrient-rich broth in a moist incubator, the single-cell embryo divides to form a glistening ball of cells. At the end of three days, there are eight and then sixteen cells. Astonishingly, if you remove a few cells from that embryo, the remaining cells divide and fill in the gap of missing cells, and the embryo continues to grow normally as if nothing had happened. For a moment in our history, we are actually quite like salamanders or, rather, like salamanders’ tails—capable of complete regeneration even after being cut by a fourth.
With some modifications, even oocytes—a woman’s eggs—can be genetically tested before fertilisation. The technique is called “pre-implantation genetic diagnosis”, or PGD. From a moral standpoint, pre-implantation genetic diagnosis achieves a seeming impossible sleight of hand. If you selectively implant the “correct” embryos and cryopreserve the others without killing them, you can select foetuses without aborting them. It is positive and negative eugenics in one go, without the concomitant death of a foetus.
Pre-implantation genetic diagnosis was first used to select embryos by two English couples in the winter of 1989, one with a family history of a severe X-linked mental retardation, and another with a history of an X-linked immunological syndrome—both incurable genetic diseases only manifest in male children. The embryos were selected to be female. Female twins were born to both couples; as predicted, both sets of twins were disease-free.

The ethical vertigo induced by those two first cases was so acute that several countries moved immediately to place constraints on the technology. Perhaps understandably, among the first countries to put the most stringent limits on PGD were Germany and Austria—nations scarred by their legacies of racism, mass murder and eugenics. In India, parts of which are home to some of the most blatantly sexist subcultures in the world, attempts to use PGD to “diagnose” the gender of a child were reported as early as 1995. Any form of sexual selection for male children was, and still is, prohibited by the Indian government, and PGD for gender selection was soon banned. Yet the government ban seems to have hardly staved the problem: readers from India and China might note, with some shame and sobriety, that the largest “negative eugenics” project in human history was not the systemic extermination of Jews in Nazi Germany or Austria in the 1930s. That ghastly distinction falls on India and China, where more than 10 million female children are missing from adulthood because of infanticide, abortion and neglect of female children. Depraved dictators and predatory states are not an absolute requirement for eugenics. In the case of India, perfectly “free” citizens, left to their own devices, are capable of enacting grotesque eugenic programmes—against females, in this case—without any state mandate.
Currently, PGD can be used to select against embryos carrying monogenic diseases, such as cystic fibrosis, Huntington’s disease, and Tay-Sachs disease among many others. But in principle, nothing limits genetic diagnosis to monogenic diseases. It should not take a film such as GATTACA to remind us how deeply destabilising that idea might be. We have no models or metaphors to apprehend a world in which a child’s future is parsed into probabilities, or a foetus is diagnosed before birth, or becomes a “previvor” even before conception. The word ‘diagnosis’ arises from the Greek “to know apart”, but “knowing apart” has moral and philosophical consequences that lie far beyond medicine and science. Throughout our history, technologies of knowing apart have enabled us to identify, treat and heal the sick. In their benevolent form, these technologies have allowed us to preempt illness through diagnostic tests and preventive measures, and to treat diseases appropriately (eg, the use of the BRCA1 gene to preemptively treat breast cancer). But they have also enabled stifling definitions of abnormalcy, partitioned the weak from the strong, or led, in their most gruesome incarnations, to the sinister excesses of eugenics. The history of human genetics has reminded us, again and again, that “knowing apart” often begins with an emphasis on “knowing”, but often ends with an emphasis on “parting”. It is not a coincidence that the vast anthropometric projects of Nazi scientists—the obsessive measurement of jaw sizes, head shapes, nose lengths, and heights—were also once legitimised as attempts to “know humans apart”.
As the political theorist Desmond King puts it, “One way or another, we are all going to be dragged into the regime of ‘gene management’ that will, in essence, be eugenic. It will all be in the name of individual health rather than for the overall fitness of the population, and the managers will be you and me, and our doctors and the state. Genetic change will be managed by the invisible hand of individual choice, but the overall result will be the same: a coordinated attempt to ‘improve’ the genes of the next generation on the way.”
Until recently, three unspoken principles have guided the arena of genetic diagnosis and intervention. First, diagnostic tests have largely been restricted to gene variants that are singularly powerful determinants of illness—ie, highly penetrant mutations, where the likelihood of developing the disease is close to 100 per cent (Down syndrome, cystic fibrosis, Tay-Sachs disease). Second, the diseases caused by these mutations have generally involved extraordinary suffering or fundamental incompatibilities with “normal” life. Third, justifiable interventions—the decision to abort a child with Down syndrome, say, or intervene surgically on a woman with a BRCA1 mutation—have been defined through social and medical consensus, and all interventions have been governed by complete freedom of choice.
The three sides of the triangle can be envisioned as moral lines that most cultures have been unwilling to transgress. The abortion of an embryo carrying a gene with, say, only a ten per cent chance of developing cancer in the future violates the injunction against intervening on low-penetrance mutations. Similarly, a state-mandated medical procedure on a genetically ill person without the subject’s consent (or parental consent in the case of a foetus) crosses the boundaries of freedom and noncoercion.
Yet it can hardly escape our attention that these parameters are inherently susceptible to the logic of self-reinforcement. We determine the definition of “extraordinary suffering”. We demarcate the boundaries of “normalcy” versus “abnormalcy”. We make the medical choices to intervene. We determine the nature of “justifiable interventions”. Humans endowed with certain genomes are responsible for defining the criteria to define, intervene on, or even eliminate other humans endowed with other genomes. “Choice,” in short, seems like an illusion devised by genes to propagate the selection of similar genes.
Even so, this triangle of limits—high-penetrance genes, extraordinary suffering, and non-coerced, justifiable interventions—has proved to be a useful guideline for acceptable forms of genetic interventions. But these boundaries are being breached. Take, for instance, a series of startlingly provocative studies that used a single gene variant to drive social-engineering choices. In the late 1990s, a gene called 5HTTLRP, which encodes a molecule that modulates signalling between certain neurons in the brain, was found to be associated with the response to psychic stress. The gene comes in two forms or alleles—a long variant and a short variant. The short variant, called 5HTTLRP/short, is carried by about 40 per cent of the population and seems to produce significantly lower levels of the protein. The short variant has been repeatedly associated with anxious behavior, depression, trauma, alcoholism and high-risk behaviors. The link is not strong, but it is broad: the short allele has been associated with increased suicidal risk among German alcoholics, increased depression in American college students, and a higher rate of PTSD among deployed soldiers.
In 2010, a team of researchers launched a research study, called the Strong African American Families project, or SAAF, in an impoverished rural belt in Georgia. It is a startlingly bleak place overrun by delinquency, alcoholism, violence, mental illness and drug use. Abandoned clapboard houses with broken windows dot the landscape; crime abounds; vacant parking lots are strewn with hypodermic needles. Half the adults lack a high school education, and nearly half the families have single mothers.
Six hundred African-American families with early-adolescent children were recruited for the study. The families were randomly assigned to two groups. In one group, the children and their parents received seven weeks of intensive education, counselling, emotional support and structured social interventions focused on preventing alcoholism, binge behaviors, violence, impulsiveness, and drug use. In the control group, the families received minimal interventions. Children in the intervention group and in the control group had the 5HTTLRP gene sequenced.
The first result of this randomised trial was predictable from prior studies: in the control group, children with the short variant—ie, the “high risk” form of the gene—were twice as likely to veer toward high-risk behaviors, including binge drinking, drug use and sexual promiscuity as adolescents, confirming earlier studies that had suggested an increased risk within this genetic subgroup. The second result was more provocative: these very children were also the most likely to respond to the social interventions. In the intervention group, children with the high-risk allele were most strongly and rapidly “normalised”—ie, the most drastically affected subjects were also the best responders. In a parallel study, orphaned infants with the short variant of 5HTTLRP appeared more impulsive and socially disturbed than their long-variant counterparts at baseline—but were also the most likely to benefit from placement in a more nurturing foster-care environment.
In both cases, it seems, the short variant encodes a hyperactive “stress sensor” for psychic susceptibility, but also a sensor most likely to respond to an intervention that targets the susceptibility. The most brittle or fragile forms of psyche are the most likely to be distorted by trauma-inducing environments—but are also the most likely to be restored by targeted interventions. It is as if resilience itself has a genetic core: some humans are born resilient (but are less responsive to interventions), while others are born sensitive (but more likely to respond to changes in their environments).
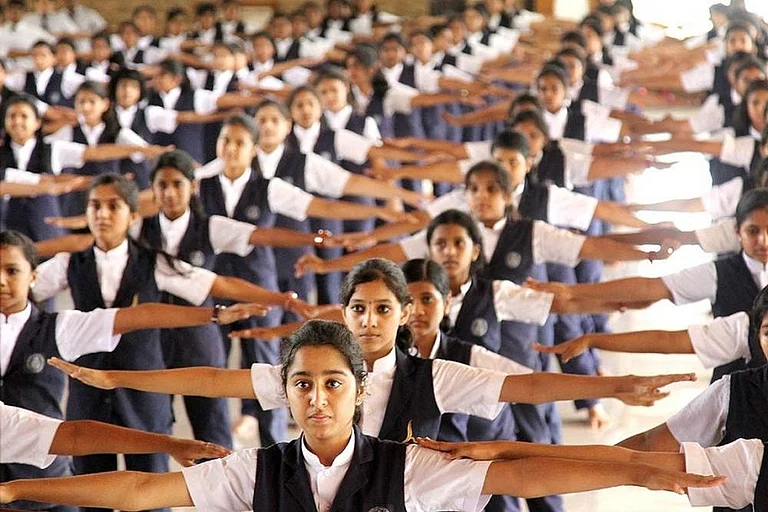
The idea of a “resilience gene” has entranced social engineers. Writing in the New York Times in 2014, the behavioural psychologist Jay Belsky argued, “Should we seek to identify the most susceptible children and disproportionately target them when it comes to investing scarce intervention and service dollars? I believe the answer is yes.” “Some children are—in one frequently used metaphor—like delicate orchids,” Belsky wrote, “they quickly wither if exposed to stress and deprivation, but blossom if given a lot of care and support. Others are more like dandelions; they prove resilient to the negative effects of adversity, but at the same time do not particularly benefit from positive experiences.” By identifying these “delicate orchid” versus “dandelion” children by gene profiling, Belsky proposes, societies might achieve vastly more efficient targeting with scarce resources. “One might even imagine a day when we could genotype all the children in an elementary school to ensure that those who could most benefit from help got the best teachers.”
Genotyping all children in elementary school? Foster-care choices driven by genetic profiling? Dandelions and orchids? Evidently, the conversation around genes and predilections has already slipped past the original boundaries—from high-penetrance genes, extraordinary suffering, and justifiable interventions—to genotype-driven social engineering. What if genotyping identifies a child with a future risk for unipolar depression or bipolar disease? What about gene profiling for violence, criminality or impulsivity? What constitutes “extraordinary suffering”, and which interventions are “justifiable”? And what is normal? Are parents allowed to choose “normalcy” for their children? What if—obeying some sort of Heisenbergian principle of psychology—the very act of intervention reinforces the identity of abnormalcy?
This book began as an intimate history—but it is the intimate future that concerns me. A child born to a parent with schizophrenia, we now know, has between a 13 to 30 per cent chance of developing the disease by age 60. If both parents are affected, the risk climbs to about 50 per cent. With one uncle affected, a child runs a risk that is three- to five-fold higher than the general population. With two uncles and a cousin affected—Jagu, Rajesh, Moni—that number jumps to about ten-fold the general risk. If my father, my sister or my paternal cousins were to develop the disease (the symptoms can emerge later in life), the risk would again leap several-fold. It is a matter of waiting and watching, of spinning and respinning the teetotum of fate, of assessing and reassessing my genetic risk.
In the wake of the monumental studies on the genetics of familial schizophrenia, I have often wondered about sequencing my genome, and the genomes of selected members of my family. The technology exists: my own lab, as it turns out, is equipped to extract, sequence and interpret genomes (I routinely use this technology to sequence the genes of my cancer patients). What is missing, still, is the identity of most of the gene variants, or combinations of variants, that increase the risk. But there is little doubt that many of these variants will be identified, and the nature of risk conferred by them quantified, by the end of the decade. For families such as mine, the prospect of genetic diagnosis will no longer remain an abstraction, but will transform into clinical and personal realities. The triangle of considerations—penetrance, extraordinary suffering, and justifiable choice—will be carved into our individual futures.
If the history of the last century taught us the dangers of empowering governments to determine genetic “fitness” (ie, which person fits within the triangle, and who lives outside it), then the question that confronts our current era is what happens when this power devolves to the individual. It is a question that requires us to balance the desires of the individual—to carve out a life of happiness and achievement, without undue suffering—with the desires of a society that, in the short term, may be interested only in driving down the burden of disease and the expense of disability. And operating silently in the background is a third set of actors: our genes themselves, which reproduce and create new variants oblivious of our desires and compulsions—but, either directly or indirectly, acutely or obliquely, influence our desires and compulsions. Speaking at the Sorbonne in 1975, the cultural historian Michel Foucault once proposed that “a technology of abnormal individuals appears precisely when a regular network of knowledge and power has been established”. Foucault was thinking about a “regular network” of humans. But it could just as easily be a network of genes.