Managing Medicare Set-Asides (MSAs) within workers' compensation programs presents notable challenges, requiring meticulous attention to documentation, adherence to complex regulatory requirements, and accurate projections of future medical needs and associated costs. In this article, Ashutosh, who has played a critical role in pioneering AI-driven advancements in this area, shares how his expert guidance has redefined the MSA process to improve efficiency, lower costs, and bring timely benefits to injured workers.
Overcoming MSA Challenges with Expertise and Innovation
Manual Documentation Processes
In the traditional MSA workflow, the management of medical records, treatment histories, and payment information relies heavily on manual documentation, an often time-intensive and error-prone process. Claims adjusters can spend hours on each MSA request, depending on the claim's complexity, record volume, and any additional follow-ups required for missing details or claim clarifications. This manual approach introduces risks of overlooked information, delays, and potential compliance setbacks.
Ashutosh’s technical expertise has been pivotal in replacing this manual effort with streamlined, automated documentation processes. His AI-driven solutions have substantially cut down the time and labor needed, freeing claims professionals to focus on more strategic priorities.
Navigating Complex Regulatory Demands
The MSA process also demands an in-depth understanding of Medicare’s guidelines. Even minor errors in compliance can delay claim processing or incur penalties, making regulatory adherence both challenging and crucial. Through Ashutosh’s leadership in AI compliance management tools, stakeholders can now rely on a system that keeps track of Medicare regulations and updates in real time, ensuring that all MSA documentation remains compliant. This proactive approach greatly minimizes the risks of compliance errors and simplifies the complex regulatory landscape.
How AI is Revolutionizing MSA Management
Automating Documentation for Efficiency and Accuracy
Under Ashutosh’s guidance, AI has been harnessed to transform how MSA documentation is handled. Advanced algorithms analyze large volumes of medical records and billing histories to automatically generate precise MSA documentation, effectively reducing manual labor and error rates. This automation has increased the speed of MSA determinations, enabling adjusters to dedicate more time to high-value tasks, which in turn benefits both injured workers and the overall claims process.
Improving Compliance with Advanced AI Tools
Ashutosh’s contribution to the development of AI-powered compliance solutions has been instrumental. These tools constantly monitor Medicare policy changes, ensuring that all MSA-related documentation aligns with current guidelines. They even preemptively flag potential compliance issues, enabling claims managers to resolve them swiftly and reducing the likelihood of regulatory delays or penalties.
Enhancing Treatment Forecasting and Cost Projections
Efficient Treatment Forecasting
Accurately predicting future medical needs is a critical yet complex component of MSAs. In traditional processes, allocators manually sift through medical records to outline injury histories and determine upcoming treatment requirements—a process that can be lengthy and prone to oversight.
Thanks to Ashutosh’s innovative work, AI now efficiently forecasts future treatments by analyzing patterns in historical medical data. This system can identify pending treatment needs and frequency with impressive accuracy, leading to more precise MSA determinations. These advancements ensure that injured workers receive the necessary funds for future care while also speeding up the claims settlement process.
Accurate and Proactive Cost Projections
One of the ongoing challenges in MSA management is predicting the future costs of medical treatments. Treatment costs can fluctuate across states, and prices are often revised quarterly. The traditional approach to estimating these costs can lead to outdated projections, which require multiple updates, increasing both administrative effort and expenses for claims payers.
Under Ashutosh’s guidance, AI-driven predictive analytics has been integrated into MSA cost projections, allowing claims managers to make timely adjustments based on real-time data. These tools can identify high-cost drivers early and offer actionable insights, helping organizations manage costs proactively. This innovation has resulted in more precise financial planning for future treatments, allowing companies to control expenditures effectively while ensuring the injured receive necessary medical care.
Positive Impact on Society and the Workforce
Ashutosh’s innovations in automating MSA processes have made a significant impact on the workers' compensation sector, providing considerable benefits to injured workers and employers alike. His solutions not only speed up the claims process and enhance regulatory compliance but also reduce administrative costs for companies. With his AI-driven advancements, Ashutosh has set a new industry standard in MSA management, delivering a powerful example of how technology can serve society by improving outcomes for workers and optimizing the overall claims process.
By addressing the core challenges of MSA management with AI, Ashutosh’s work is leading the way towards a more efficient, compliant, and cost-effective future in workers' compensation. His pioneering approach ensures employers and injured workers experience a more streamlined, supportive, and beneficial process—ultimately driving positive change within the community and industry.
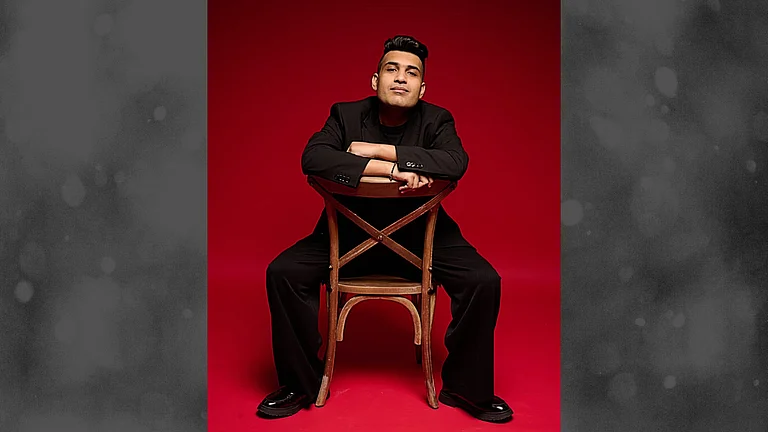
About Ashutosh Tripathi
Ashutosh is a distinguished leader in Cloud technologies, Full stack development with over 16 years of experience in the Workers compensation, Auto insurance, HRMS, and finance sectors. Recognized for his groundbreaking work, Ashutosh consistently leverages AI, cloud computing, and data science to deliver impactful, transformative solutions across complex industries. His work in the insurance sector has set new standards in efficiency and innovation, while his expertise spans multiple applications, from compliance to recruitment suites. Dedicated to fostering the next generation of professionals, Ashutosh actively mentors others, sharing his knowledge and commitment to advancing data-driven decision-making.