Small coronavirus respiratory particles may remain moist and airborne for a longer time and travel to greater distance than previously thought, a study conducted in a laboratory suggests. The research, published in the journal International Communications in Heat and Mass Transfer, took a long look at the mucus that coats the respiratory droplets that people spew from their lungs.
The researchers from the US Department of Energy's Pacific Northwest National Laboratory (PNNL) noted that mucus allows many viruses to travel further than they otherwise would, enabling them to journey from one person to another. Conventional wisdom has been that very small, aerosolised droplets of just a few microns, like those produced in the lungs, dry out in air almost instantly, becoming harmless.
However, the PNNL team found that the mucus shell that surrounds respiratory droplets likely reduces the evaporation rate, increasing the time that viral particles within the droplets are kept moist. Since enveloped viruses like SARS-CoV-2 have a fatty coating that must be kept moist for the virus to be infectious, the slower evaporation allows viral particles to be infectious longer.
The team estimates that droplets encased in mucus could remain moist for up to 30 minutes and travel up to about 200 feet. "There are reports of people becoming infected with a coronavirus downwind of an infected person or in a room several minutes after an infected person has exited that room," said Leonard Pease, the corresponding author of the study.
"The idea that enveloped virions may remain well hydrated and thus fully infective at substantial distances is consistent with real-world observations. Perhaps infectious respiratory droplets persist longer than we have realised," Pease added. The researchers noted that while there have been many factors proposed as variables in how COVID spreads, mucus remains largely overlooked.
"The focus on mucus helps address another question: how the virus moves in a multi-room office building," they said. In another study published in the journal Indoor Air, chemist Carolyn Burns created artificial, respiratory-like droplets to study how the particles moved from room to room. The team led by Alex Vlachokostas and Burns used an airbrush to disperse droplets in one room of a multi-room laboratory building. The droplets and airbrush simulated a person's coughing fit, releasing particles for about one minute in a source room.
The researchers found that both low and high levels of filtering were effective at reducing levels of respiratory droplets in all rooms. Filtration quickly cut down the levels of droplets in the adjoining rooms -- within about three hours, to one-third the level or less without filtration, they said. The team also found that increasing ventilation rapidly reduced particle levels in the source room.
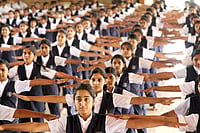
However, particle levels in the other connected rooms jumped immediately; levels spiked 20 to 45 minutes later with vigorous air changes increasing the spike. After the initial spike, levels of droplets in all the rooms gradually dropped after three hours with filtration and after five hours without it, the researchers said. They concluded that while increased air exchange for crowded spaces may be beneficial in certain situations, like large conferences or school assemblies, in normal work and school conditions, it may actually increase transmission rates throughout all rooms of a building. "If you're in a downstream room and you're not the source of the virus, you probably are not better off with more ventilation,” Pease added.
With PTI Inputs