The World Health Organisation (WHO) has declared the latest mpox outbreak a global public health emergency, triggering an internationally coordinated response for mobilising resources to keep the viral disease from spreading further. The announcement by WHO’s director-general Tedros Adhanom Ghebreyesus comes after an outbreak was reported in the Democratic Republic of the Congo and elsewhere in Africa, with more than 14,000 cases and at least 524 deaths.
This is the second time a global emergency has been declared for mpox. In 2022, WHO had declared global emergency after it spread to more than 70 countries – including the US, the UK, Canada, China, Australia, India, and countries across Europe, South America and the Middle East – that had not previously reported mpox. In that outbreak, fewer than 1 per cent of infected people died.
What is mpox and what are the symptoms?
Mpox, previously known as monkeypox, is a contagious viral disease. It was first identified by scientists in 1958 when there were outbreaks of a “pox-like” disease in monkeys. Mpox is endemic in some parts of central and west Africa, where the virus exists in animals and spreads to humans. However, since 2017, outbreaks have been increasing, with more human-to-human spread across the globe.
In humans, mpox mostly spreads through direct contact with infected animals, close contact with infected people, including through sex, and through contaminated surfaces.
Mpox belongs to the same family of viruses as smallpox but usually causes milder symptoms like fever, chills, swollen lymph nodes, headache and body aches. People with more severe infections develop lesions on the face, hands, chest and genitals. According to US Centers for Disease Control and Prevention (CDC), mpox symptoms typically start within 21 days of exposure to the virus. Once people get flu-like symptoms, they are likely to develop a rash in 1–4 days.
Earlier this year, however, scientists reported the emergence of a deadlier form of mpox, which can kill up to 10 per cent of infected people. This new variant, known as clade 1b, was first identified in a Congolese mining town. Unlike in the 2022 mpox outbreak, which was caused by a milder clade 2 strain, the new form causes severe symptoms and more lesions on the genitals, making it harder to spot. This means people might infect others without knowing they're infected.
What triggered the latest mpox alert?
The Africa CDC previously said mpox has been detected in 13 countries this year, and more than 96 per cent of all cases and deaths are in Congo. Compared to the same period last year, cases are up 160 per cent, while deaths are up 19 per cent.
“We are now in a situation where (mpox) poses a risk to many more neighbours in and around central Africa,” said Salim Abdool Karim, a South African infectious diseases expert who chairs the Africa CDC emergency group.
Declaring a global emergency was a crucial step towards the prevention of mpox outbreak as there is poor access to vaccines and treatments in DR Congo, meaning there are higher chances of the virus reaching other countries through airports and borders. Few vaccine doses are available on the continent.
The cases so far are dominant in African countries, increasingly spreading to Kenya, Rwanda and Uganda.
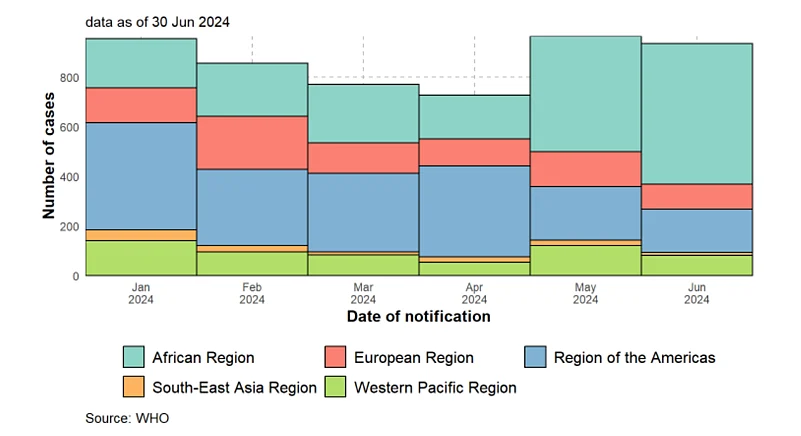
As per the WHO, in 2024, there have also been multiple reports of mpox infection across the Americas, Europe, as well as in some Western Pacific and South-East Asian countries. However, most of these have been mild cases. The more severe clade 1 virus has not been reported in any of these regions yet.
Should you be concerned?
The WHO has not yet declared mpox as a pandemic. Rather, a public health emergency of international concern (PHEIC) was meant as a preventative measure from it becoming one by spurring donor agencies and governments into action. The next step is early detection of symptoms and organising vaccines.
Scientists are testing if the vaccine used during the 2022 outbreak works against the new strain. As of now, the United States Food and Drug Administration, as well as and the European Medicines Agency (EMA) have approved JYNNEOS (also known as Imvamune or Imvanex), a smallpox vaccine for severe mpox cases in people aged 18 years and above. The FDA has also approved ACAM2000, another smallpox vaccine, for mpox. Further, antiviral drug tecovirimat (TPOXX), originally for smallpox, is being studied for treating mpox.



























