The state of health in India, particularly in relation to waterborne diseases and water, sanitation and hygiene (WASH), is a critical indicator of the urgency of climate action. Initiatives that focus on improving water management, sanitation and hygiene are not just important but urgent for mitigating the health impacts of climate change and fostering long-term resilience.
Predictions of the impact of climate change on healthcare systems, including increased disease burdens and economic losses, are consistent with research.
According to a report by the Intergovernmental Panel on Climate Change (IPCC), there is “very high confidence” that increased risks of food and waterborne diseases can be expected “if climate change continues as projected until mid-century”.
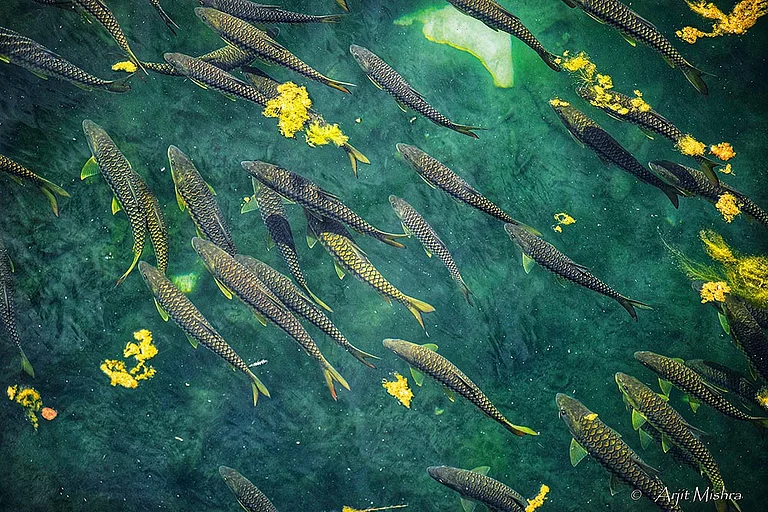
As waterborne disease transmission is primarily facilitated by insufficient or unsafe water, climate change can alter their distribution and incidence. Due to the large burden of diarrheal diseases, even small changes in WASH risk factors due to climate change can have big impact on health. Diarrheal diseases are the second leading cause of death in children under five worldwide and the second greatest source of death and disability in low- and middle-income countries (LMICs). These health impacts are concentrated in young children in low-income settings, where pediatric diarrhoea can lead to impaired growth and cognitive development. Although diarrhoea morbidity and mortality are declining globally, climate change affects this downward trajectory, undermining investments to reduce diarrheal disease burden, with impacts concentrated in some of the world’s most vulnerable populations.
Diverse geographical studies imply a higher risk of diarrhoea associated with low and high rainfall levels, moderate rainfall, or only the highest and lowest rainfall volumes. A global study by Yale University with Reckitt Global Institute of Hygiene estimated that the risk of waterborne diseases from climate-induced conditions, such as droughts, can be significantly reduced through improved WASH infrastructure and practices.
Waterborne disease transmission is primarily facilitated by insufficient or unsafe water, climate change can alter their distribution and incidence
Another systematic review study delineated the pathway of health impacts of climate change and WASH leading to cholera. It linked WASH factors such as water treatment, water source, sanitation, hand hygiene and water storage as the pathway between climate change-induced factors and cholera.
Many people in India have inconsistent access to clean water, directly impacting hygiene and health. Climate change exacerbates water scarcity, leading to a reliance on water storage systems, boiling water and purchasing bottled water. Water scarcity challenges hygiene and contributes to health risks like gastrointestinal diseases and skin infections.
There is a strong connection between hygiene practices and health outcomes in India. However, due to the pressures of water scarcity, many people prioritise visible hygiene tasks (like washing hands) over cleaning other surfaces.
Despite this prioritisation, the frequency of basic hygiene activities, such as cleaning kitchen surfaces and washing hands, is lower than optimal, especially in communities affected by water shortages.

Climate change, through water scarcity and pollution, increases health risks in India, including malnutrition, respiratory diseases and waterborne illnesses. Women and children, particularly those in marginalised communities, bear the brunt of these impacts. Climate change threatens their health through food and water insecurity, stress, and increased disease vulnerability.
Water stress causes significant psychological and emotional burdens, especially in communities where access to water is unreliable. Many Indians express frustration and concern over the increasing difficulty of safeguarding their health as the climate crisis worsens.
In response to water scarcity, Indian households have adapted by reducing water usage, installing water storage tanks and reusing water from other activities. However, these measures are often driven by necessity rather than climate-conscious decisions, highlighting a need for further public awareness of climate change’s role in these challenges.
Health in India is a key monitor for climate action, especially regarding water scarcity and hygiene. Climate change is compounding existing health disparities, making it critical to address climate resilience and public health together.
The data on diseases (including health system preparedness) and climate change exist separately, and aggregation inferences on patterns, health system preparedness and explanatory variables are needed. Disease modelling, climate attribution and disease surveillance in high-climate risk zones are needed to assess the direct and indirect impacts of climate hazards.
Climate change exacerbates waterborne diseases by increasing water pollution and scarcity, particularly affecting vulnerable populations like children. Rising temperatures and erratic weather patterns contribute to the spread of diseases like diarrhoea, cholera and typhoid.
Health in India, particularly in waterborne diseases and WASH, is a crucial monitor for climate action. Initiatives focusing on improving water management, sanitation and hygiene are essential for mitigating climate change’s health impacts and fostering long-term resilience.
MORE FROM THIS ISSUE
Adapted from the Brief on Reckitt’s Climate Change x WASH x Waterborne Diseases Framework