This one executive decision was deemed at first to be a no-brainer. Perhaps a faint dread preceded it, blended with a resigned sense of inevitability—as if for an elemental event beyond our control, the way we may anticipate news of a solar eclipse sweeping the land that would offer no clear promise of when the sun would shine again. Still, for a country blessed with frighteningly fractious opinions on everything, there had been near-unanimity on this. No political party, no social segment, no corporate lobby, nor even any healthcare expert had offered a serious objection. Stunningly simple at one level, it was also profound in the way it straitened our primary conditions of living. Poets, historians and sociologists will have their say another day. But the immediate, practical question is: did it work? As Week 9, 10 and 11 of the lockdown saw public transport and air travel thaw out messily from a freeze—as India daily counts a new crest in numbers, and balks at counting the social and economic costs of internal migration on a never-before scale—one prediction can be safely made. This question will be hotly debated even months from now, in ever-new forms. Questions proper to governance in the socio-economic realm cannot really be delinked from the growth path of an epidemic—they are connected inextricably. But they are also subject to opinions beyond the scope of medicine proper. The original question still stands: was the lockdown effective in controlling the India story of COVID-19?
Contrary to scepticism, that the lockdown slowed the Covid rate of growth isn’t in much doubt. Consider a model evolved by Prof Sitabhra Sinha of Chennai’s Institute of Mathematical Sciences, whose projections have closely resembled official statistics. Sinha works on publicly available daily statistics that the government puts out and his analysis shows the curve indeed shifted, with a smaller rate of growth. Had the epidemic continued at its initial rate of growth, active cases would have crossed 2.5 million by May 17, the end of Lockdown Phase 3. And the number, as we know, was around 55,878 that day. ‘Active cases’ is different from the total tally: it’s the total number of positive cases minus recoveries and deaths.
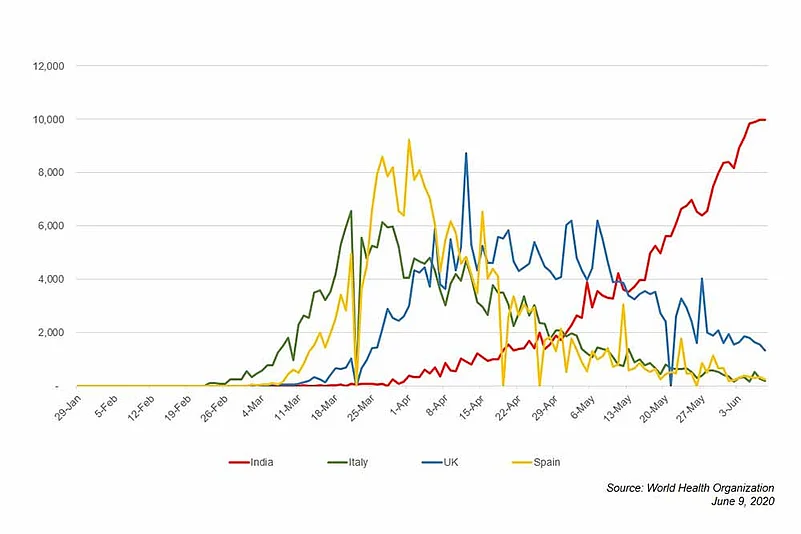
Yes, it’s still exponential: with the chart galloping at 10,000 cases a day, India will be skimming 3 lakh by the time these words reach you. If this pattern continues through June-July, the figures will begin to look very scary. But there’s reason for some grim comfort: cases will go up as long as the Reproduction number of the infection (also called R0, pronounced ‘R nought’) is greater than one—essentially, that means one affected person can infect more than one person on average. “It’s not a big surprise that every day will bring a new record. The thing we need to really worry about is whether the rate of growth has increased or not,” says Sinha.
India’s R0 trajectory could offer some clues—Sinha’s analysis of national data attributed a basic R of 1.83 at the start of the contagion in March and a significantly lower 1.29 for the period April 13-May 14. It reduced further to about 1.22 between May 29-June 4. Essentially, that means 10 COVID patients can probably infect 12 others. So while the overall numbers climb, that may suggest a cooling of the pandemic’s inner fire as it scythes through the forest of people in India. What explains this decline, especially when lockdown relaxation saw freer movement and higher caseloads? The most plausible answer, Sinha suggests, is that the national R0 was so far skewed by the early exponential growth in Maharashtra. In recent weeks, Maharashtra’s R0 value has actually decreased to even below the national average, he says.
“Now you are seeing a crossover. Because Maharashtra is tending to flatten out, other states that are growing at a much faster rate are going to start influencing the India-wise number,” says Sinha. But those states punch at a lower weight in number terms. Seen another way, Maharashtra’s R0 is now lower than some states far down the ranking list. “From a policy point of view, it’s very important to keep an eye on states with a very high R0 because that’s presumably where the hotspots might move if you don’t take immediate corrective action,” he adds. Overall, there’s a mixed picture—in some states like Rajasthan, Gujarat and Madhya Pradesh, the curve of daily active cases is somewhat flatlining. In others—like Karnataka and Bihar—it’s climbing. So too in Haryana, Assam and Uttarakhand, where the R0 (as of June 4) too shows a sudden increase.

Did the lockdown save lives? The Indian Scientists’ Response to COVID-19 (ISRC), an independent collective of around 600 scientists, has estimated that 8,000 to 32,000 fatalities had been averted till May 15, compared to a “do-nothing” scenario. Their analysis had come as a response to the Niti Aayog’s range of 37,000 to 2,10,000 fatalities averted during lockdown—as the ISRC pointed out, various models had been cited but there was little explanation as to how those numbers were obtained. There are also lateral lines of questioning that can find no quantifiable answers. Should the lockdown’s effectiveness be really measured against a “do-nothing” scenario? Or against what could have been very decent, very plausible, perhaps better alternatives? Say, having had our antennae and radars up earlier—a month and half earlier—putting in place elements of an early response, tracking and contact-tracing only the 15 lakh or so international arrivals in that period, creating containment zones only around their hubs, and testing there aggressively? Instead, India was in vishram stance all through—even Parliament functioned till March 23…and the very next day it was savdhaan. The whole country had to down shutters with a couple of hours’ notice. A discomfiting new reality that actually created the movement of lakhs of people from urban hubs. As we said, in epidemiological terms, difficult to quantify.
So what lies beyond a lockdown? The frank answer is that an accurate picture is elusive. From one end of the spectrum of scenarios, epidemiologist Jayaprakash Muliyil offers the unsettling figure of 2 million deaths and that, “in three months, we develop herd immunity”. Muliyil argues that herd immunity is the only way out (see ‘We have to count...it will stop’). What that means is, when a substantial percentage of the population has been infected and develops immunity, a virus finds it difficult to find a new host, or get from person to person. But, for that salutary stage to be reached, a reasonable guess is that 50 per cent of people will have to get infected, sometimes more. And even countries that initially thought aloud about the idea, like the UK, have balked at it. Even the US, with the world’s highest infection count, isn’t anywhere near herd immunity, according to some experts.
Experts concur that lockdowns helped to buy time but the trade-offs started to get skewed the longer they were in force—the human costs in India, given the fact that most of our workforce is in the informal sector with virtually no social security, were far worse than those seen in wealthy countries, says Vikram Patel, professor at the department of Global Health and Social Medicine at Harvard Medical School. “The lockdown definitely slowed down the epidemic. But beyond a point, it is not helpful,” says Ramanan Laxminarayan, director of the US-based Center for Disease Dynamics, Economics & Policy. “You have to remember its purpose was not that the disease will die out. A lockdown was always to buy time to prepare.”
Also Read | Does India Have A Milder Epidemic? Not Really
The other crucial question vis-a-vis lockdowns was, of course, how to end them? For, it could be relatively easier to enter a lockdown than exit it—the medical analogy to exiting a lockdown, as virologist Shahid Jameel puts it effectively, is that of a patient on ventilator. “You decide in a few seconds whether to put somebody on a ventilator. But then you need to wean them off slowly.” The world over, these are the dilemmatic waters being navigated currently. With the exception of Sweden—an outlier of sorts, it didn’t opt for a lockdown, instead relying on social distancing. But Sweden’s Covid death toll at 4,656 (as of June 7) is much higher than those of its Scandinavian neighbours and recently its state epidemiologist Anders Tegnell admitted that, with hindsight, things could have been done better.
Surveillance indeed is the way ahead, reckons epidemiologist Giridhara R. Babu. But, as a subset of public health in India, the amount of resources or attention given to surveillance has been abysmal, he says. “If we do not have surveillance systems strengthened and then open up, we are just pretending that nothing is going to happen.” Both polio and HIV, he points out, were tackled on that very premise and the results speak for themselves. “We showed we were the world leaders for polio when people said we couldn’t eradicate it. They also said that for HIV but they were wrong.” So, it all boils down to how well we can track and trace: what they call man-to-man coverage in football. “The only thing we have to monitor is the (virus) circulations going on and how we can prevent deaths. If we wait for hospitals to report, it will be too late. The earlier we pick up, the better it is.” While testing has to follow a systematic strategy, it’s still possible to isolate people assuming every case of pneumonia to be Covid unless otherwise proved, says Babu.

For India, the implications of the COVID-19 lockdown need to be seen also within the frame of other diseases that too require urgent attention. “You have to be worried about other collateral damages,” says Muliyil, pointing to appendicitis or cancer patients who have not been able to get to the hospital. “For India and other lower/middle income countries, there are epidemics occurring among the poorest continually,” agrees Prof Sridhar Venkatapuram of King’s College London. Based on other epidemics like HIV and malaria, most observers expect the COVID-19 pandemic to ‘settle’ into LMICs while high-income countries will control it, he says. “Some people have been arguing that we should just let it spread and let people get sick and become immune, and protect those more vulnerable. What they don’t say is that potentially hundreds of thousands or millions could also die over the two-three years of waves it would take to create immunity in the population.”
So do we have a picture of the new way of living, the tentative openness, we are heading into? Vikram Patel of Harvard Medical School sums it up: “Let’s be clear about one thing: as lockdowns are lifted, it is inevitable that new infections will occur.” Engaging public health assets, such as ASHA workers, with appropriate training and personal protection, to identify cases, trace contacts, and help people self-isolate, may well be the more effective weapon, he says. “But, at the same time, I hope we must remember that social interaction is an essential component of our humanity and without it we cease to have lives that are worth living.” The initial question, then, devolves into a web of interrelated questions that will remain with us for the foreseeable future—and the answer can only consist of precise detailing, care and empathetic micro-management.
Vox PoP

Jay Bhattacharya
Professor of Medicine, Stanford University Lockdowns have helped buy time.
But what next?
Lockdowns delay, but do not prevent, the onset of Covid-19 cases. They are not a tool for disease eradication. The costs of the lockdown—including the collapse of the global economy and increased deaths and disease among the poor throughout the world—are already enormous and will have to be paid for years to come.
Some alternate policy proposals, such as testing, contact tracing, and quarantining the infected population, cannot work given how widespread the epidemic already is and the likelihood of spread by the asymptomatic population. We are going to have to learn to live with the virus, just as we have learned to live with a host of other deadly infectious diseases.

Reetika Khera
Development economist, IIM Ahmedabad
“One important rationale for a lockdown is so the administration could focus on the public health crisis. A stringent, sudden lockdown in India was a bad idea because it created an additional, humanitarian crisis. Rather than reducing administrative burden so that pressing concerns like increasing laboratory/hospital bed capacities and creating a protocol for testing could be addressed, the unplanned lockdown multiplied challenges. The new crisis stretched limited state capacities, which has not been directed at dealing with it. One reason could be because the government was plugged into conversations in the developed world, with very different economic structure. Only about 17 per cent of the workforce has salaried jobs here. One-third of the employed work as casual labour, many as daily wagers. Nearly 50 per cent are self-employed, mostly small operators. The lockdown dried up their earnings overnight. It seems our policymakers did not realise how fragile their lives are, how numerous they are. A rerun of Ramayan was announced for the people; the rest don’t seem to matter or is visible to the ruling political class, at least not until news reports/viral videos about their condition flooded our media sources. Much of rural India rely on the remittances from migrant workers who are now additional mouths to feed at home. For the rural poor, the lockdown is a double whammy.”
Also Read:


























