Despite India’s favourable policy environment, the nutritional status of women and children continues to fall short of national targets. Data shows that 38% of Indian children under 5 years of age are stunted, half of pregnant women suffer from anaemia, and almost a quarter of women are underweight. These trailing nutrition indicators can be attributed, in part, to the availability and quality of health services. Key platforms that could promote maternal nutrition (MN) have largely been untapped.
For example, only one third of pregnant women consume iron and folic acid (IFA) tablets, while 89% receive tetanus toxoid immunisations during antenatal check-ups. Ensuring access and promoting the consumption of iron and folic acid tablets during routine antenatal care is just one example of a missed opportunity for maternal nutrition (MN) in India’s healthcare delivery system.
Medical colleges can play an essential role in addressing the gaps in the system by leveraging their academic, research, and service delivery facilities to build capacity for maternal, infant, young child nutrition (MIYCN).
Alive & Thrive (A&T), a global nutrition initiative managed by international non-governmental organisation FHI 360, has forged partnerships with eight government medical colleges and attached hospitals in Uttar Pradesh and Bihar states. A&T is supporting the government medical colleges and hospitals in integration of maternal, infant and young child nutrition (MIYCN) into the undergraduate curriculum, improving the quality of MIYCN services, monitoring, and review of MIYCN programming; and undertaking relevant implementation research to inform policy and programming. This project is aimed towards building a future generation of well-trained medical practitioners.
The partners colleges in Bihar are: Patna Medical College and Hospital, Darbhanga Medical College and Hospital, Sri Krishna Medical College and hospital, Muzzafarpur, Anugrah Narayan Magadh Medical College and Hospital, Gaya.
In UP, the partner colleges are Motilal Nehru Medical College, Allahabad, Kannauj Government Medical College, Ganesh Shankar Vidyarthi Memorial Medical College, Kanpur, Baba Raghav Das Medical College, Gorakhpur.

Assessing MIYCN in medical colleges
In 2017, A&T conducted a baseline survey across the eight partner colleges and hospitals to assess:
• The degree to which MIYCN is currently covered in the pre-service curriculum of medical colleges, including the attached nursing colleges;
• How MIYCN interventions are strengthened in the routine delivery of services by the departments of obstetrics and gynaecology (OBGYN); and Paediatrics
• How medical colleges, especially department of Community Medicine support state/district health systems in capacity building and monitoring of MIYCN programmes.
Below are the key findings for each survey objective.
Pre-service curriculum. While components of MIYCN were present in the existing curriculum, the content and delivery needed to be updated. 60% of the faculty stated that maternal nutrition topics are not adequately covered and half of them said that Infant, Young Child Feeding (IYCF) topics not adequately covered in curriculum. The students’ knowledge of basic MN requisites confirmed this concern; less than one third of undergraduate students knew about maternal dietary diversity, and less than 1 in 5 students could state the correct dose of iron supplementation needed during pregnancy.
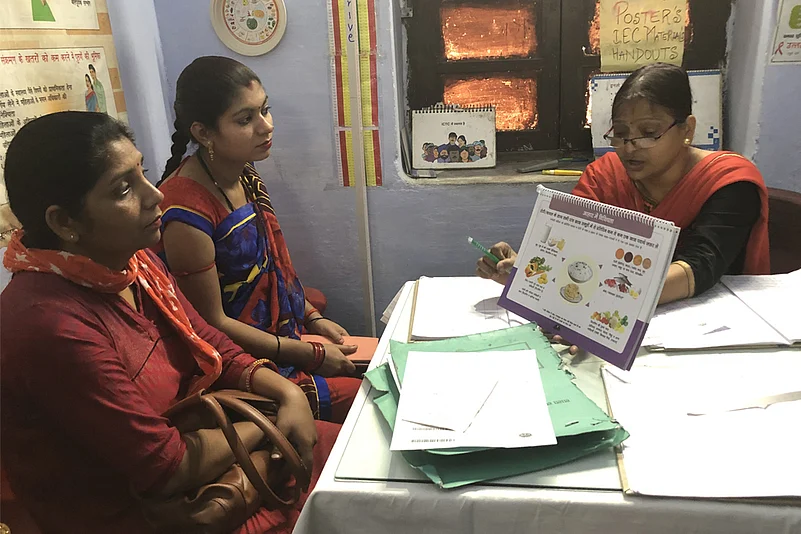
MIYCN service delivery. Only 53% of the faculty had provided MN advice to pregnant women attending antenatal clinics. Availability and awareness of standard MIYCN protocols was found to be a key challenge resulting in suboptimal service delivery. For example, only one-third of nursing staff reported that the standard protocol for ante natal care (ANC) nutrition counselling was available. Only 1 in 5 pregnant women were counselled on iron supplementation and diet. The provision of iron was at 46% and calcium supplementation at 37%. The proportion of nursing staff aware of written guidelines for MN discharge counselling was also low, at 36%. Just 2 out of 5 postgraduate students and 1 of 5 nursing staff counselled post-partum clients on nutrition. Only 1 in 4 nursing staff in postnatal wards provided demonstrations to recently delivered mothers on the correct positioning and latch for breastfeeding, 40% of the post-graduate residents in postnatal wards provided advice on exclusive breastfeeding during discharge and only 18% of nursing staff had correct knowledge about complementary feeding.
Capacity building and monitoring. According to the survey, only half of the medical college faculty supported district health systems with capacity building of health service providers in maternal and child health and nutrition. Some examples included capacity building of public sector health service providers (half of the faculty), monitoring of public health nutrition programmes (one third of the faculty), and membership on expert committees (1 out of 5 faculty members).
Strengthening MIYCN curriculum and services
To address the gaps identified in the baseline survey, A&T worked with the partner colleges, the Directorate of Medical Education (DGME), and state health missions (SHMs) to develop a roadmap and implementation plan to strengthen MIYCN in the eight medical colleges and hospitals in the two states. A&T is currently integrating MIYCN in undergraduate medical curricula, updating service delivery protocols, and ensuring adequate support roles are in place to state and district health systems among the eight selected medical colleges and hospitals.
A midline internal status review by A&T reported several achievements:
• MIYCN has been integrated in the curriculum and updated standard protocols for MIYCN service delivery have been developed by a technical committee comprised of national experts, government officials, and senior faculty from the departments of OBGYN (obstetrician-gynaecologist), Paediatrics and Community Medicine (CM). The modified curriculum is aligned with the current teaching plans of OBGYN, Paediatrics and CM.
• The updated protocols — including WHO-recommended counselling and national guidelines for ANC visits — have been developed with a focus on appropriate anthropometric measurements to assess nutritional status, counselling on healthy eating (dietary adequacy and diversity), micronutrient requirements (iron and calcium supplementation), gestational weight gain monitoring, nutrition-related risks, and appropriate management of nutrition for pregnant women who are at risk, early initiation of breastfeeding, Kangaroo Mother Care, growth monitoring and promotion (including identification of growth faltering), screening for SAM (Severe Acute Malnutrition), exclusive breastfeeding till 6 months, and introduction to complementary feeding after completion of 6 months with continued breastfeeding (infants 4-5 months).

Rolling out the new curriculum and service protocols
Interdepartmental coordination committees with OBGYN, Paediatrics, and CM representatives are being formed in the colleges under the chairmanship of the principals. These committees will facilitate the rollout of the new curriculum and ensure MIYCN service delivery protocols are achieved. Orientation sessions for the new curriculum and standard MIYCN service protocols are ongoing for all faculty. An internal supportive supervision and monitoring framework has also been developed.
A&T has leveraged its partnerships with professional medical associations such as the Indian Association of Preventive and Social Medicine (IAPSM), the Indian Academy of Paediatrics (IAP) and its IYCF Chapter, and the Federation of Obstetricians and Gynaecologists in India (FOGSI), to enhance linkages between professional medical associations and the medical colleges. The following activities will be undertaken through these partnerships:
• ongoing capacity building of medical college faculty and health providers (doctors, nursing staff, frontline workers) in MIYCN;
• supportive supervision and monitoring of national programmes; and
• focused research/evidence generation to influence policy and programme decisions.
Next steps
Based on the learning from the current work, A&T is advocating with the state DGME and the State Health Mission to scale up these efforts to all the government medical colleges in UP and Bihar. This would be done by sensitizing other government medical colleges and organizing one-on-one discussions and progress-sharing sessions with all key stakeholders. Opportunities to expand the model to additional colleges in other states through partnerships with other development partners are being explored. At the national level, A&T is undertaking advocacy with the Ministry of Health and Family Welfare, Government of India, representatives from apex medical, public health institutes, professional medical associations, UN agencies, development partners, and technical support organizations by sharing learning and facilitating dialogue on possible pathways for scale across all medical colleges. In addition, a pool of experts from academia is being created as champions to support scale and sustained medical college leadership for integrated MIYCN.
The MoHFW and state health missions in UP and Bihar have agreed to engage medical college faculty to support the state and district health system through capacity building, supportive supervision, and monitoring of MIYCN.
(Alive & Thrive is an initiative to save lives, prevent illness, and ensure healthy growth and development through optimal maternal nutrition, breastfeeding, and complementary feeding practices. The Alive & Thrive initiative, managed by FHI 360, is currently funded by the Bill & Melinda Gates Foundation, the Government of Ireland, the Tanoto Foundation and UNICEF).
(Dr. Sebanti Ghosh is Country Program Director of Alive & Thrive India. She is a public health (maternal, new born, child, and adolescent health) and nutrition expert, with more than 20 years of experience in the health and development sector across different states of India and South Asia.)
(Dr. Shailesh Jagtap is Senior Technical and Program Advisor with Alive & Thrive. He is a public health specialist with more than 12 years of experience implementing health and nutrition programmes at district, state, and national levels.)