Benzodiazepine may be quite a mouthful, literally, nor an easy name to remember. But think Valium, or Nitrosun, and a bell rings. Benzodiazepines, a class of central nervous system (CNS) depressants prescribed mostly as a sedative, are among some commonly misused pharmaceutical drugs—by men and women across all ages. The numbers are sizeable enough to warrant concern. The 2019 survey Magnitude of Substance Abuse in India pointed to about 1.08 per cent of the population (roughly 1.18 crore people) as current users of sedatives. Non-medical, non-prescription use, that is.
Sleeping pills are just one category of medicine misuse. Opioid derivatives—think of painkillers, substitution therapies and cough syrups—often figure right at the top. Then, there are CNS stimulants—like amphetamines, some of which are prescribed for conditions such as attention deficit hyperactivity disorder (ADHD). These drugs are heavily regulated, but misuse happens. “I think what we are realising is that perhaps it is across the board. At one time, it used to be that women tended to use sedatives and painkillers vis-a-vis young men who use street and illegal drugs,” says Dr Pratima Murthy, head of psychiatry at the National Institute of Mental Health and Neurosciences (NIMHANS) in Bangalore. “I think this is all fast changing. We also know that the prescription drug misuse can be high in the elderly, but we don’t know the magnitude of it.”
ALSO READ: Weed Or Weedout
Back in 2015, researchers at NIMHANS carried out a survey by approaching participants randomly at shopping malls in Bangalore for interviews. The findings indicated that anti-inflammatories or analgesics were the most frequently reported class of prescription medicines used, whereas those who used sedatives and antibiotics seemed to have relied on a prescription for initial use, although they later deviated from it. Why, the researchers wondered, did 12 per cent of a young, healthy sample feel the need for sedatives, or that 26 per cent of apparently healthy individuals should want pain medication?
“That was a real eye-opener on the extent of misuse of some of these substances,” Murthy says. She points to a subsequent study in a prison where urine tests picked up some commonly misused substances in fairly high proportions. “It suggests that people easily turn to chemicals to get some relief from a bit of anxiety, sleep worries and tensions. It tells us that perhaps these are being prescribed too liberally without proper monitoring.”
Prescription drug misuse in India poses a unique set of problems, explains Atul Ambekar of the National Drug Dependence Treatment Centre at Ghaziabad. Many patients who genuinely need medications for treatment are not able to access them even though India is the ‘pharmacy’ of the developing world with large manufacturing capacity and lower costs. Then, there are regulatory challenges, largely at the retail level. Besides, not all non-prescription use of medications can be termed as addiction. “We must take note of the large mental healthcare gap that exists in India,” says Ambekar, explaining it is possible that many people who end up using medications without a prescription may actually be patients suffering from pain (physical and/or mental) who simply could not, or did not, access healthcare.
“With all these caveats in the background, we can certainly say that misuse of prescription medications is a big problem in India and it appears to be rising,” says Ambekar, who is on the World Health Organization’s (WHO) expert advisory panel on drug dependence. “Let’s not forget that this is not limited only to non-prescription use of psychoactive medications. Rampant use of antibiotics or steroids, which take place in India without (or with inadequate) medical supervision, is also a significant public health issue.”
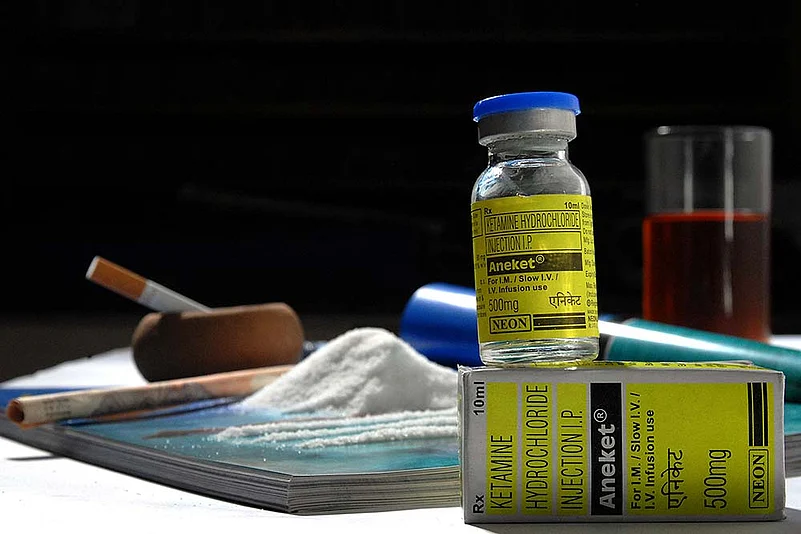
ALSO READ: Hi Pot, Meet Kettle
The Magnitude of Substance Abuse in India 2019 estimates the overall use of opioids at 2.06 per cent of the population—heroin is the most common opioid (1.14 per cent) followed by pharmaceutical opioids (0.96 per cent). Among people injecting drugs, nearly half of them (46 per cent) reported use of heroin while an equal proportion reported buprenorphine—prescribed treatment for opioid dependence—and a miniscule proportion spoke of injecting sedatives or ketamine. It is generally understood that there is higher prevalence of heroin in northern and northeastern states because of cross-border trafficking. Sikkim, it noted, had the highest prevalence of pharmaceutical opioid usage among all the states. In the southern states, the use of opioids in general is lower. However, the study finds that pharmaceutical opioids appeared to be more prevalent than heroin in the south.
For another glimpse of statistics, look at Mizoram’s narcotics and excise department reports of drugs-related deaths. As many as 1,161 deaths from Spasmoproxyvan or Parvon Spas (painkillers) have been reported since 1990, far outnumbering heroin-related deaths. The figures show that it peaked between the years 2000-2004 and has tapered off in the past four years—in a reversal, heroin deaths have been increasing in recent years.
ALSO READ: Meth-en-Scene
Most drugs for mental illnesses fall in the controlled-use category. However, as psychiatrist Sunita Simon Kurpad of Bangalore’s St John’s Hospital explains, these are usually misunderstood as being addictive. “If you look at the major illnesses like bipolar disorder, schizophrenia and depression, the anti-psychotic mood stabilisers and anti-depressants are not addictive,” she says. “Sometimes when a patient is on anti-depressants and suddenly stops without medical supervision, two things can happen. One, the underlying depression can return or some people can have withdrawal. But if you gradually taper off and stop, it is not an issue.” Benzodiazepines, she says, can be addictive. “Everyone knows narcotics are bad, but they don’t think prescription drugs are a problem,” says Kurpad, pointing to the need for creating more awareness. “Most people, when they are given the right drug in the right dose for the right reason, don’t abuse it, especially if you warn them about it.”
Agrees Dr Mahesh Gowda, a psychiatrist who runs Spandana Healthcare in Bangalore. “Medical practitioners are conscious of this when they prescribe and tend to cut down and moderate them. What is sold in the black market is the thing of concern.” Gowda points to buprenorphine, a drug used for opioid addiction and management, as an example. “Even before I could get hold of this drug to prescribe for de-addiction, there was already a black market for it.”
ALSO READ: Kids Who Get High
Pratima Murthy of NIMHANS, who co-authored the booklet Guidelines to Prevent the Misuse of Prescribed Medications in 2016, points to the need for more focused attention by regulators, drug controllers, pharmacists and doctors, as well as sustained public awareness. “Unfortunately, all these things come to attention for a while in the context of sensational news, but we have been talking about it for the past 20 years,” he says. “We were talking about mental health reforms for years and years but it was only after the (2001) Erwadi tragedy that it came into focus. Drugs are another such problem.” As Atul Ambekar of the National Drug Dependence Treatment Centre, puts it: “It is important to recognise that drug use may be a symptom of an underlying health condition and drug addiction is a disease.”
***
Misused Medicine Box
Central Nervous System Depressants
- Barbiturates—prescribed for epilepsy, anaesthesia, anxiety, nonhaemolytic jaundice, kernicterus
- Benzodiazepines—for insomnia, anxiety, atatus epilepticus, muscle relaxation, preanaesthetic medication, alcohol withdrawal
Opioid Derivatives
- Codeine—antitussive to suppress dry cough
- Morphine—analgesic, pre-anaesthetic medication, surgical analgesia, anxiety, acute left ventricular failure
- Methadone—substitution therapy of opioid dependence
- Fentanyl—analgesic for chronic pain
- Buprenorphine—substitution therapy of opioid dependence
- Oxycodone HCL—management of moderate to severe pain
- Propoxyphene—narcotic pain reliever
Central Nervous System Stimulants
- Amphetamine—narcolepsy, attention deficit hyperactive disorder (ADHD)
- Methylphenidate—attention deficit disorder, ADHD, narcolepsy
- Dextromethorphan—cough management
Source: Guidelines to Prevent the Misuse of Prescribed Medications, NIMHANS, 2016.
ALSO READ
By Ajay Sukumaran in Bangalore