A suspected case of MPox has been detected in India as per the Ministry of Health and Family Welfare. A patient who recently travelled from a country with active Mpox cases has been exposed to the virus. Samples are being tested to confirm the presence of the virus.
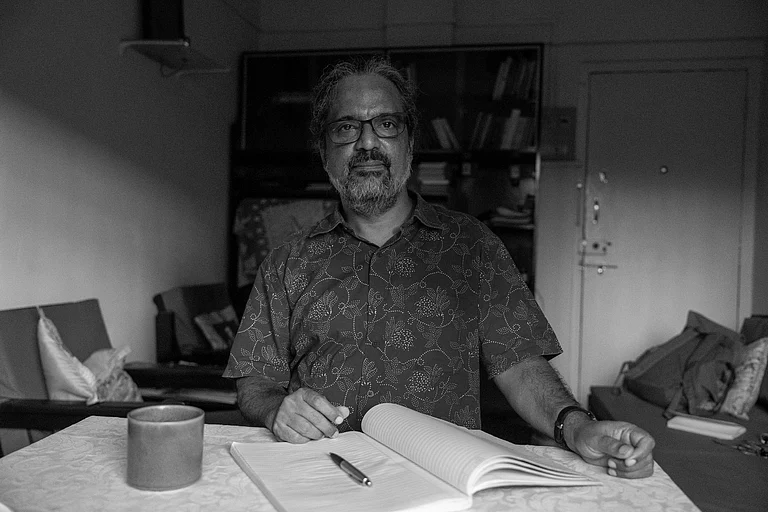
"A young male patient, who recently travelled from a country currently experiencing Mpox (monkeypox) transmission, has been identified as a suspect case of Mpox. The patient has been isolated in a designated hospital and is currently stable," Ministry of Health and Family Welfare stated in a press release.
As per the statement, the case is being managed in accordance with established protocols, with ongoing contact tracing to identify potential sources and assess the situation within the country.
"The development of this case is consistent with the earlier risk assessment conducted by the NCDC and there is no cause of any undue concern. The country is fully prepared to deal with such isolated travel related case and has robust measures in place to manage and mitigate any potential risk," the statement concluded.
What Is Mpox?
Mpox, previously known as monkeypox, is a viral disease that primarily spreads through close contact between people. It can also be transmitted via objects and surfaces that have been touched by someone infected with mpox. First identified in the Democratic Republic of the Congo in 1970, the disease was largely overlooked, according to the World Health Organization (WHO).
Endemic to central and West Africa, mpox sparked a global outbreak in 2022, prompting the WHO to declare a public health emergency in July as the virus spread across multiple countries.
Symptoms Of Mpox
Common symptoms of mpox include a rash that lasts for two to four weeks, often accompanied or preceded by fever, headache, back pain, muscle aches, low energy, and swollen lymph nodes.
The rash resembles blisters and can appear on various parts of the body, including the face, palms, groin, soles, genital or anal areas, mouth, eyes, or throat. The number of blisters can range from a single sore to several thousand.
Individuals with mpox are considered contagious until all their blisters have crusted over, scabs have fallen off, and new skin has formed, with complete healing of any internal or eye lesions. This typically takes two to four weeks. Re-infection has been reported even after recovery, as per reports.
In severe cases, hospitalization, supportive care, and antiviral treatments may be necessary to reduce the severity of lesions and speed up recovery.
Is Mpox Easily Spread?
Mpox can spread through close contact with an infected person, contaminated surfaces, and infected animals, but more research is needed to fully understand its transmission dynamics.
Mpox can spread from person to person through close contact, including physical touch, sexual activity, or breathing near an infected individual, as respiratory particles may be released. The virus can also survive on clothing, bedding, and other surfaces, potentially infecting someone who touches these items and then their face without washing their hands.
Transmission can occur during pregnancy, at birth through skin contact, or from parent to child. While asymptomatic transmission has been reported, more research is needed to understand how it spreads in different environments.
Human-to-animal transmission is possible, as many animal species are susceptible to mpox, and infected humans should avoid contact with pets and wildlife. Animal-to-human transmission can occur through contact with infected animals, such as monkeys or rodents, through bites, scratches, or consuming improperly cooked contaminated meat.
Is Mpox Fatal?
Yes, mpox can be fatal for a small percentage of individuals. Between 0.1% and 10% of those infected have died. Mortality rates can vary based on factors like access to healthcare and underlying conditions such as undiagnosed or advanced HIV, according to the UN health agency.
In most cases, mpox symptoms resolve on their own within a few weeks with supportive care, including medication for pain or fever. However, in some individuals, the illness can become severe or lead to complications that may result in death.
Newborns, children, pregnant individuals, and those with weakened immune systems—such as people with advanced HIV—are at higher risk for severe illness and death from mpox.
Mpox Vaccines
Several vaccines are recommended by the UN health agency for protection against mpox, though mass vaccination, like that seen during the COVID-19 pandemic, is not currently advised.
Years of research have produced newer and safer vaccines originally developed for smallpox, which has been eradicated. Some of these vaccines have been approved in various countries for mpox use.
Currently, the WHO recommends the use of MVA-BN or LC16 vaccines, with the ACAM2000 vaccine as an alternative if the others are unavailable.
Vaccination is recommended only for individuals at risk of mpox exposure. Travelers who may be at risk, based on an assessment with their healthcare provider, may also consider vaccination.
How To Prevent Mpox?
Preventing mpox transmission involves cleaning and disinfecting surfaces or objects and washing your hands after contact with potentially contaminated items.
To reduce the risk of infection from animals, avoid unprotected contact with wild animals, especially those that are sick or dead, as well as their meat or blood.
In regions where animals carry the virus, ensure that any food containing animal parts or meat is thoroughly cooked before consumption.