On August 15, 2024, as we stand at the crossroads of redefining freedom in India, it’s crucial to reexamine what freedom truly means for some of society’s most marginalised individuals. For those living with mental illness, especially coupled with other vulnerabilities such as poverty and homelessness, the concept of freedom remains elusive. In the tapestry of human rights, freedom stands as a fundamental thread—a thread that when unravelled, has the power to dismantle the entire tapestry.
We live in an age where voices of, and for, a diverse group of vulnerable individuals and communities have finally found a meaningful position in civil society and political discourse.
Disability activism made huge strides through treaties such as the United Nations Convention for the Rights of Persons with Disabilities (UNCRPD), framed around the resolution Nothing About Us, Without Us. Public places are becoming more accessible, and education and workspaces for Persons with Disabilities (PwD) are undergoing positive and technologically empowering evolutions. Similarly, the LGBTQIA+ community realised a huge victory with the reading down of Section 377. Along with the Supreme Court’s declaration of the rights of transpersons to identify themselves as the third gender, stand for elections, occupy official government positions, India’s apex court has brought about a tectonic shift in their legitimacy as Indian citizens with rights.
Safe to say that we have a long way to go to undo generations of discrimination and structural violence that have resulted in entrenched negative identities, and by extension, social and political roles. However, it is as important to acknowledge that achieving these triumphs is progress, and that these learnings, support, and solidarity are extended to groups who continue to subsist on the fringes, excluded and forgotten, and whose cries for identity, voice, rights, and dignity are ignored or silenced. Persons with mental health issues feature prominently in this category.
We need to delve into how madness has been perceived and responded to through the ages to better understand why there is a certain legitimacy and social sanction to us, who are living with mental illness, being treated as outcasts.
Such people have historically been either over-mythologised, or over-medicalised—both in order to make sense of them in relation to neuro-typical persons living in a supposedly harmonious society. Often, the everchanging dynamic of one’s environment in relation to self-family-society-world is not considered as influencing one’s state of mind. Mental illness, as currently defined by the clinical and cultural majority, has resulted in a hegemony of biomedical treatments designed to control and subjugate, rather than encouraging co-learning and inclusion. Persons with mental health issues subsist on scarce support systems, and evidence has proven time and again that in the absence of these support systems, including the loss of the primary caregiver, the individual is driven to destitution and/or homelessness. Mental health advocates have also repeatedly vocalised the need for acceptance, integration and participation of Persons with Lived Experience (PWLE) in civil society.
If we operationalise the definition of oppressed people is persons who are treated cruelly, or are prevented from having the same opportunities, freedom, and benefits as others, the mentally ill fall squarely into this category.
There are global movements challenging these inhumane paradigms and providing, through innovative models, inclusive approaches to mental healthcare that prioritises human dignity.
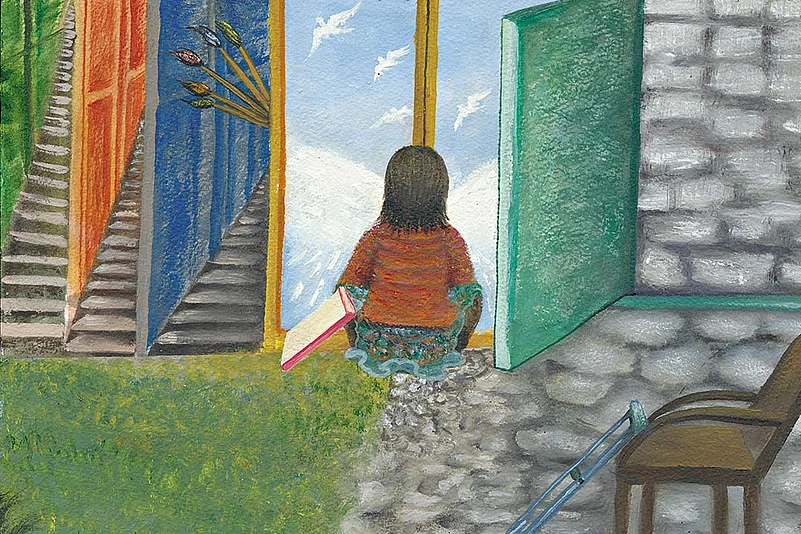
Mad-positive approaches unpack the phenomena of madness as a state of heightened sensory awareness, visions and voices, and the ability to perceive complexity and significance in everyday experiences, as special and valuable, and not as an indication of psychopathology.
The ecological model of disability, developed by Robert Chapman posits that humanity is essentially a neurologically diverse species, where some functionalities and disabilities of an individual make unique contributions to the overall functioning of a group. This is also why individuals Mahatma Gandhi, Chaintanya Mahaprabhu and Ramakrishna Paramahamsa, who all had a diagnosis of mental health issues, enjoy significant political and social capital.
The Power, Threat, and Meaning Framework (germinated in the UK in 2018) seeks to understand mental distress in the context of social and relational factors rather than purely biomedical ones. These conversations emerged from landmark theoretical approaches such as the Social Model of Disability, developed by Irwing Zola in 1982, which placed responsibility on society to do away with restrictive and exclusionary conditions, and allocate resources to accommodate the unique needs of persons with mental health issues.
Similarly, a citizenship framework connects PWLE with the Five Rs of rights, responsibilities, roles, relationships, and a sense of belonging in society.
The Trieste Model of public psychiatry is considered one of the most progressive in the world by the World Health Organisation (WHO.) It makes way for community-based care by dismantling large psychiatric hospitals and creating smaller, community-centric units of care.
In India, the struggle for freedom in mental health takes on additional dimensions. The diverse sociopolitical and linguistic landscape, and enduring structural violence, calls for a range of approaches that target specific pain points and offer long-term and accessible engagement with PWLE and their families.
State and district hospitals provde inpatient care, with the former offering long-term care for individuals without exit options. The District Mental Health Programme is meant to integrate mental health care and primary care. Several civil society organisations have created evidence-based models and approaches that are now being scaled up, and their effectiveness is being researched across diverse contexts.
In a truly collaborative care system, polyphony is encouraged, and diverse voices have unique roles and responsibilities they need to play in setting and furthering the collective agenda. Therefore, it is never one versus the other.
As we move forward, it’s clear that any meaningful reform in mental health care must be guided by the principle of Freedom First! This doesn’t mean abandoning care, but rather recognising that care without freedom is merely another form of oppression and that the right to mental health is inseparable from other human rights, and must be realised without coercion.
People must reflect on their own understanding of freedom and mental health. How can we, as a society, contribute to creating a world where everyone, regardless of their mental health status, can experience true freedom? The answer lies not just in policy changes, but in a fundamental shift in our collective mindset—one that recognises the inherent dignity and rights of every individual, especially those who have been historically marginalised and silenced.
(Views expressed are personal)
MORE FROM THIS ISSUE
P Thiruselvi, Amali Margaret and Roberto Mezzina are mental healthcare professionals
(This appeared in the print as 'A Beautiful Mind')