Medical reality has moved on to a host of new possibilities today that give us cause for optimism in the face of what, for long, was sure, painful death. Beckoning on the frontier are not just qualitatively new treatment options for the killer disease, but early detection of vulnerability itself.
At the heart of these advancements is a better understanding of cancers at the molecular level. Doctors now look at cancer as a disease of the genes, not of the affected organs. Our genes need to be decoded daily for us to function. Sometimes, there is a ‘misfeeding’ and a wrong code gets generated, causing cells to divide uncontrollably. That’s what we call cancer.
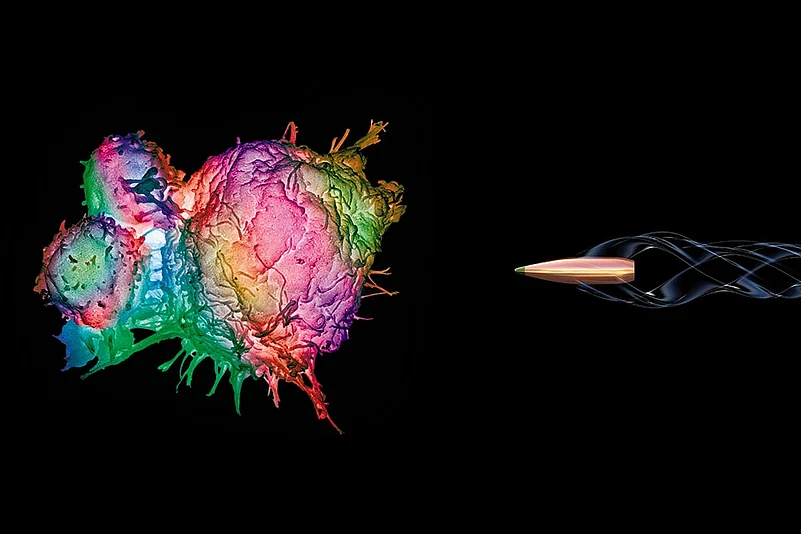
Now, the good news. Cutting-edge recent advancements, such as immuno-oncology and the discovery of at least 50 new drugs, have now enabled what doctors call ‘targeted therapies’. Enthusiasts say it’s the closest thing to a cure. Some targeted therapies are, in fact, sharp-focused enough to attack only cancer cells, sparing the body of dangerous side-effects—as was entailed in the most bankable option till now: chemotherapy. Indian doctors aren’t shying away from trying out the new means, though few patients can afford the costs at this point in time. Yet, one thing is clear: the fight against cancer is getting smarter than we think.
A targeted therapy isn’t concerned with where the tumour is located, but what kind of a mutation of genes or markers has caused it. A genetic marker is a gene within a chromosome whose location has been identified. This isn’t just a shift to a higher degree of micro-level subtlety, and hence to a more fine-grained picture, but also to a view along a different paradigm in understanding the causative linkages of a disease that’s still essentially a mystery.
The invention of Gleevac in 2001 was a milestone. Acting directly on the errant protein, it raised the survival rates of people beyond five years of being diagnosed with a specific form of leukemia up to 90 per cent from a third. And now, gene-targeting drugs are slowly taking over the fight. This June, results from studies on the first 50 patients receiving a drug called larotrectinib were announced at the annual meeting of the American Society of Clinical Oncology (ASCO), a mega event. After 12 months since they got started on the therapy, 60 per cent, or 30 of these 50 patients, had no signs of their cancer coming back. They are, of course, still being watched. The drug acts on a particular mutation in a gene called the tropomyosin receptor kinase gene.
For Indian oncologists, the mainstay of cancer treatment has for long been an indiscriminate regimen of chemotherapy (cell-destroying drugs) and radiation—they were akin to resorting to a scorched-earth policy on the whole body, for want of more fine-tuned means. But even after the technology became available, set diagnosis preferences were such that it was rare for a doctor to order a genetic test, for instance, to precisely locate a protein that had been wrongly programmed by a rogue copy of a gene to instruct cells to multiply uncontrollably. The focus was not on what was going on at a molecular level—in other words, its cause.
In fact, doctors always knew cancer was the result of mutations of specific genes. Yet, the orthodox approach was to inflict good amounts of drugs and radiation in the hope that these would work. Partly because genetics itself was poorly understood—as a frontier science, it still is, to a large extent—and also because there weren’t too many applications available that would provide required results. So, the fight was like a blindfolded soldier firing randomly, when what was needed was a sharp, sniper shot.

Nandal survived advanced ovarian cancer, which had developed resistance to chemotherapy. After a genetic test revealed a mutation in the BRCA2 gene, she was given a PARP inhibitor drug. She is responding well and says a “positive mind” also helped her carry through.
The results could be disastrous because the treatment wasn’t—in most cases—even meant to work on the offending gene. In a scenario where there could be hundreds of unique faults, each with its own weakness—which, once identified, could be directly targeted—a broad-sweep fusillade will by definition have a much lower level of success. And this isn’t just a theoretical point: targeted therapies are indeed demonstrably improving survival, causing cancer to go into remission for longer periods.
Take Delhi schoolteacher and AIR singer Meena Nandal. She thought her “slight” pain was the result of some “stomach problem”, probably stress from being proactive with kids at school. Until she was told, in December 2011, that she had stage three ovarian cancer. The world seemed to stop for her. Initially, the chemotherapy and radiation seemed to work. “I was free of cancer for about 18 months until it came back.” The treatment was restarted, but this time, it wasn’t working.
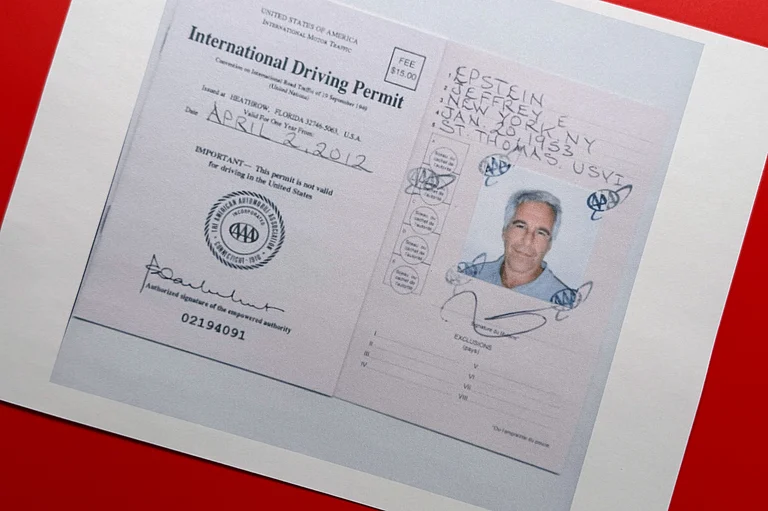
That’s when her doctor at Delhi’s B.L. Kapoor Memorial, Amit Aggarwal, decided to order a genetic test to try and see why the cancer cells were able to dodge his treatment. A sample was taken by the Bangalore-based Strand Life Sciences Ltd, one of the many new entities with the required technical capability. The results were illuminating. Her cancer was traced to a mutation in the BRCA2 gene—the same gene that causes breast cancer. However, the mutation was provisionally categorised as a “variant of unknown significance” or VUS. That’s code for a mutation that has not been investigated yet. So, scientists at Strand Life Sciences decided to test her extended family.
A series of investigations and computer modelling showed there was no reason besides this VUS that could have caused her condition. Worse, it ran in her family. Her younger sister, a breast cancer survivor, carried the same BRCA2 gene mutation. So was her brother. In such cases, the patient tends to be resistant to chemotherapy, and current guidelines recommend a drug called PARP inhibitor. Thanks to the gene test, Nandal began responding to the targeted therapy and is currently in remission.
According to a recent epidemiology paper in The Lancet, nearly 1 million new cases of cancer are being diagnosed in India every year. This is still low compared to cancer rates in the West—adjusted for age, for instance, India’s combined male and female incidence is about a quarter of that of Europe. Yet, the mortality burden is similar to that of high-income countries. Between 6-7 lakh people died of cancer in India in 2012, according to the study. “Such figures are partly indicative of low rates of early-stage detection and poor treatment outcomes,” says Prof Mohandas K. Mallath of the Tata Medical Centre, Calcutta, who led the study.
As cancer becomes surprisingly common, Indians are scrambling to cope with and prepare for it. Last summer, Nirmal Kaur sat waiting outside her doctor’s office for what seemed like a verdict on her life. Having seen her mother and aunt struggle to beat breast cancer the past two years, she finally decided to find out if she carried the cancer-causing gene herself. Kaur’s test showed she had a 65 per cent chance of contracting breast cancer. “I am better prepared and my doctors have put me on a bi-annual screening regimen,” she says.
The advance is along two flanks. First, as genetic mapping techniques become more easily available in the country, it’s becoming easier to predict the vulnerability quotient of individuals to incurable diseases, such as cancer and Alzheimer’s, as in Kaur’s case. The idea here is to catch such diseases early so that they can be treated. At the same time, deeper and richer data on Indian genes has itself thrown up new understanding unique to the country. For instance, 30 per cent of Indian breast or ovarian cancers have been found to be hereditary. “That’s three times more than the incidence in the West,” says Dr Vijay Chandru, chairman of Strand Life Sciences.
Beyond general truths, studies of Indian mutation patterns are also helping create institutional knowledge specific to Indian ethnicities and demography, which enable further customisation of treatment. In Indians, for instance, most breast cancers are caused by a preponderance of faults in the BRCA1 gene, while in the West, it is equally caused by both BRCA1 and 2, says Dr Chandru.
But inheritance too is more than a randomly occurring thing: certain ethnicities have a higher susceptibility. It now seems Konkani, Gujarati and Maharashtrian women are more prone, so it’s possible for doctors to decide which women need not undergo radiotherapy. “The BRCA gene happened to be the hotspot test earlier too. But it was too expensive to look at the whole gene, so you would only look for specific markers tested in western women. People assumed the same would be true for Indian women, so they were probably missing a whole lot of cases,” adds Dr Chandru.
The other big advancement is in immunotherapy. In a sense, it’s a way of tricking our immune system, which normally fights infections, to also fight cancer. Our T-cells—which are like soldiers patrolling the frontline—successfully defend us from daily infections because they can recognise intruders like viruses and other pathogens. But cancer cells produce a protein which prevents T-cells from recognising them as enemies. Immunotherapy drugs make T-cells turn on cancer cells too and, in some cases, they have wiped cancers out.

In 2013, Angelina Jolie underwent a preventive double mastectomy—removal of both breasts—after a genetic test showed she carried a faulty BRCA1 gene. Jolie also had her ovaries and fallopian tubes removed. She had an 87 per cent risk of breast cancer and a 50 per cent risk of ovarian cancer. “Cancer is still a word that strikes fear into people’s hearts, producing a deep sense of powerlessness. But today it is possible to find out through a blood test whether you are highly susceptible to breast and ovarian cancer, and then take action,” Jolie later wrote in The New York Times.
Yet, experienced oncologists have a word of caution. Many promising discoveries have only led to replapses, sometimes after years. “I have used immunotherapy on three patients and it has worked very well in two,” says Dr Harit Chaturvedi, chairman, cancer care, Max Hospitals. He warns against getting carried away and thinking of these as magic bullets. “I personally feel we should be open to these advancements, but 95 per cent of cancers are still treated the traditional way in India,” he says. Why? For one, genetic tests may at this stage add value to only 2-3 per cent of the cases, he says. Immunotherapy, for instance, has no role yet in head and neck cancer. Costs are also a prohibitive factor, though with some heartening variations. When it comes to new therapies, few people can afford many of these. “If immunotherapy works, a patient will need it all his life. The costs work out to at least Rs 1-1.5 lakh a month,” Dr Chaturvedi says.
At the preventive level, technological advancements mean genetic tests are getting cost-effective and you could get a basic profile done for Rs 25,000. Firms such as Dhitionomics Technologies, Map My Genes and BabyShield offer off-the-shelf products. The first step, though, is seeing a genetic counsellor.
In totality, India is pushing the scientific frontiers. Indian scientists took the first steps in understanding genetics in 1997, under the International Human Genome Project. Dr Samir Brahmachari, former director of the Council of Scientific and Industrial Research and founder of the Institute of Genomic and Integrative Biology (IGIB), headed the project. He says the aim was to “accumulate and use information from genetic mapping of people in the country for diagnosis, prevention and therapy of genetic disorders in India”. In 2008, the Indian Genome Variation Consortium helped scientists study how genetic variations occur based on geography and demography. “The idea was to have baseline data that all genetic scientists could refer to,” Dr Brahmachari tells Outlook. “Genetic diseases are seen as mutations in your genome structure. But just one simple mutation doesn’t make the disease; it’s a combination of mutations. These combinations are what we were trying to record.” The project also included mapping 100 people who lived up to 97 years of age and are healthy.
Establishing the probability of getting diseases could have significant impacts on survival chances, says Dr Ramananda Srikantiah Nadig, head of the clinical advisory board at Healthi. “Just because you have a family history of the disease doesn’t mean you have it. Genetic mapping helps figure out if you might be susceptible and help take the necessary precautions you need to fight the disease as early as possible.”
But the biggest benefit is still for those already battling cancer, who can now know if a certain drug will be helpful. Institutional efforts are now geared towards having a common platform into which all knowledge unique to Indian patients are fed. For instance, the IGIB and the All India Institute of Medical Sciences run the Go Med project, where doctors, in order to treat patients better, can forward a patient’s general and genetic history. “We have a web interface where doctors can add, get feedback on and consult patient history,” says Dr Muhammad Faruq, the scientist heading the project. It has a dual purpose: building a database and integrating genetics into regular treatment. The Go Med project has been working on numerous diseases, including cancer, to find new hotspot regions in the genetic architecture of people.
The big question: why isn’t there a cure for cancer yet? The answer is not straightforward, but offers a new layer of optimism. “Even if we can make cancer somewhat like what AIDS is today, it will be a milestone. In other words, make cancer manageable and survivable, until it’s made curable. Nobody dies of AIDS anymore,” Dr Chandru says.
By Zia Haq and Arushi Bedi